24 Y/O Female with CSOM and Moderate Anemia
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
24 years old female student came to OPD with C/C of SOB on exertion since 1 year.
Generalised weakness since 6 months.
Easy fatiguability since 6 months. Decreased appetite since 3 months.
HOPI:
Patient was apparently
asymptomatic 1 year back then she developed SOB on exertion insidious in onset, gradually progressive from grade 1 to grade 2 (mmrc). No history of orthopnea, PND.
No H/O giddiness, occasionally palpitations present.
Generalised weakness since 6 months. Easy fatiguability since 6 months.
No H/O chest pain, pedal edema, pain abdomen, loose stools, vomitings. Decrease in appetite since 3 months. H/o poor nutritional intake.
No H/O similar complaints in past.
Past History:
- N/K/C/O DM, HTN, Asthma, CAD, CVA, TB, Epilepsy
- No H/O previous blood transfusions
Personal History:
- Appetite- Decreased
- Diet: Mixed
- Sleep: Adequate
- Bowel and bladder movements: Regular
- No addictions
Family History: Not significant
Menstrual History:
- AOM: 12 yrs
- Cycle: 3/28 normal flow
- 2-3 pads per day
- No clots
General Examination:
- Patient is C/C/C
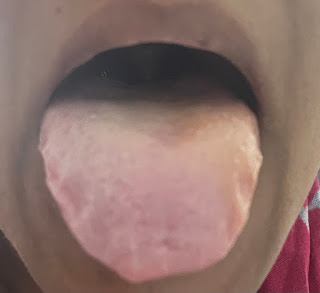
- Pallor present
- Icterus, Cyanosis, Clubbing, Lymphadenopathy, Edema absent
Vitals:
- Temp: 96.8 F
- Bp: 110/70 mmHg
- PR: 96 bpm
- RR: 18 cpm
- SpO2: 98% on RA
- GRBS: 96 mg%
Systemic examination:
- Cvs: S1 S2 +,no murmurs
- R/s: BLAE+, NVBS
- P/A soft, non-tender
- CNS: GCS E4V5M6
Investigations:
- HAEMOGLOBIN: 6.7 gm/dl
- TOTAL COUNT: 4,600 cells/cumm
- NEUTROPHILS: 50%
- LYMPHOCYTES: 40%
- EOSINOPHILS: 04%
- MONOCYTES: 06%
- BASOPHILS: 00%
- PLATELET COUNT: 5.66 lakhs/cumm
- SMEAR: Microcytic hypochromic anemia with thrombocytosis
PROVISIONAL DIAGNOSIS :
RIGHT SIDED CSOM WITH MODERATE ANEMIA
TREATMENT:
19/05/2023
1. INJ. IRON SUCROSE (200mg) 1 amp in 100 ml NS IV/OD
2. INJ OPTINEURON 1 amp in 100 ml NS IV/OD
3. MONITOR VITALS AND INFORM SOS
20/05/2023
1. TAB. OROFER-XT PO/OD @ 9 PM
2. MONITOR VITALS AND INFORM SOS
21/05/2023
1. TAB. MVT PO/OD @ 2 PM
2. MONITOR VITALS AND INFORM SOS
Case Discussion:
Project PLAR : Unexplained microcytic hypochromic anemia overtreated with iv iron
[5/19, 9:34 AM] Dr. Rakesh Biswas: What was her shortness of breath subjectivity like before today?
[5/19, 10:31 AM] Dr. Meesum Abbas: She said that she had shortness of breath on brisk walking sir
[5/19, 2:11 PM] Dr. Rakesh Biswas: So kind of nyha 2? Now asymptomatic because she can't do any brisk walking here?
[5/19, 2:22 PM] Dr. Meesum Abbas: Yes sir grade 2
[5/19, 2:24 PM] Dr. Meesum Abbas: We can check after rectifying the anemia sir, if she still has the symptoms
[5/19, 2:25 PM] Dr. Rakesh Biswas: Why does she have anemia? What's the root cause?
What's the connection with csom?
[5/19/23, 2:28:53 PM] Dr. Meesum Abbas: She gave history of reduced appetite sir. So maybe it’s nutritional
[5/19/23, 2:30:55 PM] Dr. Biswas Sir GM KIMS: How does nutritional anemia happen?
Share some evidence based literature on nutritional anemia proven with nutritional correlation data
[5/19/23, 2:33:41 PM] Dr. Meesum Abbas: Maybe the CSOM pain radiated to the TMJ and caused difficultly in mastication sir. Hence reduced appetite and anemia
[5/19/23, 2:35:03 PM] Dr. Biswas Sir GM KIMS: Out of the box 👏👏👏
[5/19/23, 2:44:04 PM] Muskaan KIMS: But she isn't complaining of any jaw pain .
[5/19/23, 2:54:07 PM] Dr. Biswas Sir GM KIMS: We are also contesting the nutritional hypothesis itself
[5/19/23, 2:54:09 PM] Dr. Meesum Abbas: Maybe it’s a general sense of sickness and discomfort because of which she had less appetite
[5/19/23, 5:01:07 PM] Dr. Prachethan: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8640113/
P-This study was conducted to determine the association between IDA and the incidence of CSOM in children.
I-All participants were examined for serum iron (FE), hemoglobin (Hb), total iron-binding capacity (TIBC), and ferritin
C-Participants were divided into case group which are children diagnosed with CSOM (n = 42) and control group which are children with normal ear
O-Iron deficiency anemia increases 3.3 times risk of CSOM in children compared to normal. Therefore, iron deficiency anemia should be considered in children with CSOM so that the treatment and prevention of CSOM can be carried out thoroughly.
[5/20/23, 7:48:49 AM] Dr. Biswas Sir GM KIMS: Please share O again in terms of absolute numbers. Like instead of saying 3 times increase, tell us the prevalence of anemia in both groups (are both n=42?) and how did they remove or tackle selection bias?
[5/20/23, 3:26:22 PM] Dr. Prachethan: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8640113/
P-This study was conducted to determine the association between IDA and the incidence of CSOM in children.
I-All participants were examined for serum iron (FE), hemoglobin (Hb), total iron-binding capacity (TIBC), and ferritin
C-Participants were divided into case group which are children diagnosed with CSOM (n = 42) and control group which are children with normal ear
O-Many researchers have identified several risk factors for CSOM, but iron deficiency has never been considered a risk factor. In this study, 31% of the case group had IDA while in the control group, 11.9% had IDA and the correlation was statistically significant with p = 0.033 and OR = 3.3.






Comments
Post a Comment