75 year female patient with hypovolemic shock( under evaluation) , type 1 respiratory failure and severe metabolic acidosis
- This is online E log book to discuss our patient’s de-identified health data shared after taking his/her guardian’s signed informed consent.
- Here we discuss our individual patient's problems through a series of inputs from an available global online community of experts with an aim to solve those patient's clinical problems with collective, current, best evidence based inputs.
- This e-log book also reflects my patient centered online learning portfolio and your valuable inputs in the comment box is welcome
Case discussion of a 75 y/o Female with Hypovolemic Shock
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment
NAME : MEESUM ABBAS
ROLL.NO : 82
BATCH : 2017
CHIEF COMPLAINT
A 75 year old female patient was brought to the casualty with chief complaints of
FEVER since 4 days .
GENERALISED WEAKNESS since 3 days .
VOMITING since 3 days .
SHORTNESS OF BREATH since 1 day.
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 3 months back and is able to do her regular work at home.
Then she developed shortness of breath of grade 3 along with dizziness and generalised weakness which made her to fall for which she was taken to a local hospital in hyderbad and used medications for the above. There were no similar episodes when on medications.
4 days back she developed fever which was low grade , intermittent, not associated with chills and rigor , no diurnal variation , relieved on medications. 2 days back she developed vomitings of 4 episodes which were non projectile , food particles as content , non bilious , non foul smelling and associated with loss of appetite ( patient's attender gives the history that she often forgets to eat food ) not associated with loose stools and pain abdomen.
She developed shortness of breath which was grade 3 not associated with chest pain , palpitations, orthopnea and paroxysmal nocturnal dyspnea .
PAST HISTORY
No similar compliants in the past and no previous hospitalisation.
Not a known case of diabetes , hypertension, asthma , Tuberculosis and epilepsy.
No past surgeries and blood transfusion.
PERSONAL HISTORY
Appetite is decreased.
Mixed diet.
Sleep adequate .
Bowel and bladder regular .
No known food and drug allergies.
No addictions.
FAMILY HISTORY
Not significant.
GENERAL EXAMINATION
* The patient is conscious , non coherent and non -cooperative .
* Moderately built and moderately nourished.
Examined the patient in supine position and in well lit room.
* Pallor : Absent
* Icterus : Absent
* Cyanosis : Absent
* Clubbing : Absent
* Lymphadenopathy : Absent
* Edema : Bilateral, pitting type upto thighs
VITALS
Temp: Afebrile
PR: 78 Beats per minute , low volume pulse , normal character and rythmn and vessel wall normal .
BP: could not be measured.
RR: 28 cycles per minute.
Spo2 - 50% at Room air. 85% at 15 litres of oxygen.
GRBS- 43 mg/dL.
SYSTEMIC EXAMINATION
* RESPIRATORY SYSTEM : Normal Vesicular Breath Sounds Audible, Position of trachea is central, Bilateral air entry present
* CVS : S1 and S2 Heard, no murmurs, no thrills
* CNS : Higher mental functions normal , Cranial nerves: intact, No meningeal signs, GCS- 15/15 , deep tendon reflexes are normal , sensory system intact.
* PER ABDOMEN : scaphoid shape, Abdomen not distended with no scars, sinuses, engorged veins , No tenderness, No palpable mass, normal hernial orifices , Bowel sounds heard.
ELECTROCARDIOGRAM
HEMOGRAM
RENAL FUNCTION TEST
BLOOD SUGAR AND BLOOD UREA
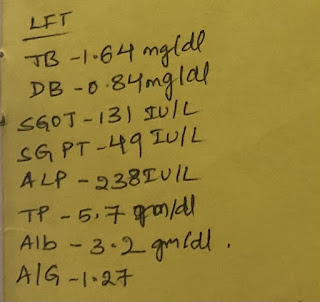
LIVER FUNCTION TEST
ATRIAL BLOOD GAS
CXR-
CARDIOMEGALY
DIFFERENTIAL DIAGNOSIS
TOXIC
INGESTION
STARVATION KETOACIDOSIS
HYPOVOLEMIC SHOCK/CARDIOGENIC SHOCK with TYPE 1 RESPIRATORY FAILURE AND SEVERE METABOLIC ACIDOSIS.
PATHOGENESIS
TREATMENT
1. 30 Normal saline bolus i.v.
2. 10 Normal saline infusion at 100ml/hr.
3. Injection Nor adrenaline ( 20mg + 30ml Normal saline ) at 8ml/hr. Increase or decrease the dose as required to maintain mean arterial pressure more than 65mm of Hg .
4. Oxygen inhalation to maintain saturation
5. Patient was intubated around 7.30 pm on 11/01/2022













Comments
Post a Comment